The Gut–Estrogen Connection in Perimenopause and Menopause
During perimenopause and menopause, many women experience symptoms that are often attributed solely to hormonal change, including bloating, constipation, breast tenderness, mood shifts, headaches, or symptoms described as “estrogen dominant.” While estrogen fluctuations and decline are part of the transition, hormone production is only one side of the equation.
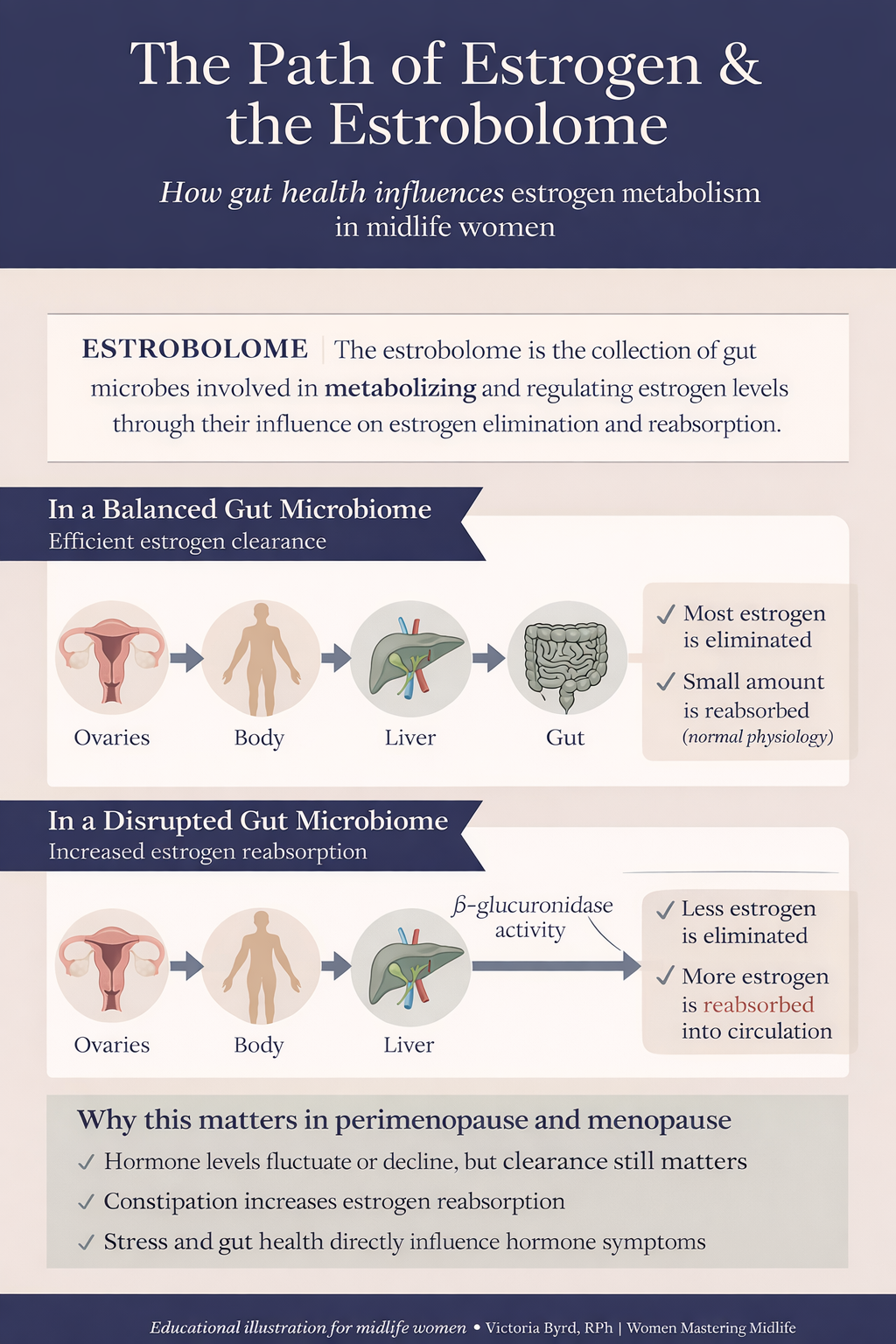
Equally important is how estrogen is metabolized and eliminated, a process that relies heavily on gut function and the gut microbiome.
As a pharmacist working with midlife women, I frequently see estrogen metabolism overlooked in clinical conversations. Understanding the gut–estrogen connection provides a more complete framework for addressing symptoms that persist despite lifestyle changes or normal laboratory results.
Estrogen Metabolism: An Overview
Estrogen metabolism is a multi-step physiological process involving both the liver and the gastrointestinal tract:
Estrogen is produced and circulates in the bloodstream
The liver modifies estrogen through conjugation, preparing it for excretion
Estrogen metabolites are secreted into bile and enter the digestive tract
The gut microbiome influences whether estrogen is eliminated in stool or reabsorbed into circulation
The final step, which occurs in the gut, is particularly relevant during midlife.
The Estrobolome and Estrogen Regulation
The estrobolome refers to the subset of gut bacteria involved in estrogen metabolism. These bacteria produce enzymes, most notably β-glucuronidase, which can deconjugate estrogen metabolites in the intestine.
When β-glucuronidase activity is elevated, estrogen that was prepared for elimination may be reabsorbed back into circulation. When gut microbial balance and bowel regularity are optimal, estrogen is more likely to be eliminated efficiently.
Research has demonstrated associations between gut microbial diversity and circulating estrogen levels in both premenopausal and postmenopausal women, supporting the clinical relevance of this pathway.
Why the Gut–Estrogen Connection Becomes More Relevant in Midlife
Perimenopause is characterized by fluctuating estrogen levels rather than a linear decline. After menopause, estrogen production shifts away from ovarian sources and depends more heavily on peripheral conversion.
At the same time, midlife is often associated with physiological and lifestyle factors that affect gut health, including:
• Reduced gut microbial diversity with age
• Slower gastrointestinal motility and increased constipation
• Higher chronic stress exposure
• Cumulative antibiotic use across the lifespan
When intestinal transit time slows or microbial balance is disrupted, estrogen metabolites remain in the gut longer, increasing the opportunity for reabsorption. This helps explain why some women experience estrogen-sensitive symptoms even when measured estrogen levels are low or declining.
In these cases, impaired estrogen clearance, rather than excess estrogen production, may be contributing to symptoms.
Clinical Patterns That May Suggest Impaired Estrogen Clearance
While no symptom is diagnostic on its own, patterns commonly observed in midlife women include:
• Constipation or infrequent bowel movements
• Persistent bloating
• Breast tenderness or swelling
• Heavy or prolonged bleeding during perimenopause
• Headaches or migraines associated with hormonal shifts
• Symptoms that worsen during periods of stress or disrupted sleep
These symptoms are multifactorial, but gut health can significantly influence their severity and persistence.
Supporting Estrogen Metabolism Through Gut Health
Supporting estrogen metabolism does not require detox protocols or restrictive interventions. The focus is on supporting normal physiology.
Dietary Fiber Intake
Dietary fiber supports regular bowel movements and helps bind estrogen metabolites in the gut, facilitating elimination. Observational studies have shown associations between higher fiber intake and lower circulating estrogen levels in postmenopausal women.
Fiber-rich foods include vegetables, legumes, whole grains, chia seeds, and ground flaxseed.
Gut Microbial Diversity
A diverse intake of plant foods supports microbial diversity. Polyphenol-rich foods such as berries, leafy greens, olive oil, herbs, and legumes are associated with beneficial microbiome activity.
Consistency is more important than dietary perfection.
Bowel Regularity
Regular elimination is essential for estrogen clearance. Hydration, adequate fiber, daily movement, and stress regulation are foundational strategies. Persistent or painful constipation should be evaluated clinically.
Probiotics: Individualized Use
Probiotics may benefit certain gastrointestinal symptoms, but they are not universally indicated and do not replace dietary and lifestyle foundations. Their role in estrogen metabolism is strain-specific and individualized.
Stress and Sleep
Chronic stress affects gut motility, intestinal permeability, and microbiome composition through the gut–brain axis. Poor sleep and elevated cortisol can indirectly impair estrogen clearance, making stress management a core component of midlife hormone support.
Key Takeaway
Estrogen balance in perimenopause and menopause is not determined solely by hormone production or laboratory values. Efficient estrogen metabolism depends on liver function, gut health, microbial balance, and regular elimination.
Supporting these systems through evidence-based nutrition and lifestyle strategies can meaningfully influence symptom management and overall well-being during the menopause transition.
If you want help mapping your GI health and working to improve your microbiome, schedule a free discovery call and we can discuss how working together, we can create health habits and labs that may help you understand your current gut landscape. https://www.womenmasteringmidlife.com/booknow
References
Flores R, et al. Fecal microbial determinants of systemic estrogen metabolites in postmenopausal women. Journal of Clinical Endocrinology & Metabolism. 2012.
https://academic.oup.com/jcem/article/97/6/2109/2836037
Kwa M, et al. The intestinal microbiome and estrogen receptor–positive breast cancer. Journal of the National Cancer Institute. 2016.
https://academic.oup.com/jnci/article/108/8/djw029/2412592
Monroe KR, et al. Dietary fiber intake and circulating estrogen concentrations in postmenopausal women. Cancer Epidemiology, Biomarkers & Prevention. 2017.
https://aacrjournals.org/cebp/article/26/7/1041/71739
Rose DP, et al. Dietary fiber and estrogen metabolism. American Journal of Clinical Nutrition. 1991.
https://academic.oup.com/ajcn/article/54/4/659/4694586
National Institutes of Health. Gut microbiome research updates.
https://www.nih.gov/news-events/nih-research-matters/gut-microbiome
The Menopause Society. Menopause education and physiology.
https://menopause.org